Survival of the safest: The protective nervous system Part 3.
In this series we are looking at pain as a protective survival response. Without pain, our life expectancy is greatly reduced. We have evolved with survival as our priority, which outweighs happiness and comfort. Unfortunately, our pain response sometimes becomes exaggerated and unreliable when we develop chronic pain.
In part 1 and part 2 we discussed what chronic pain is and how it develops. In this blog, we look at how to treat it. In my experience of working with chronic pain, treatment broadly falls into four overlapping stages: finding the right support, reframing the pain, reconditioning your body and trusting the process.
Several years ago, I had a lower back disc injury resulting in leg nerve pain. I initially noticed tingling and some odd sensations after some weightlifting, which progressed into a deep, burning ache that turned into chronic pain.
After several months, I went for an MRI, which confirmed nerve compression from a lumbar disc. As I have seen many patients with debilitating pain from similar injuries, this only alarmed me further.
Regrettably, I did not seek the right support.
1. Find the right support
There’s nothing more confusing or frustrating than receiving different messages about your pain or how to treat it from multiple therapists. If you have a multi-disciplinary team supporting you, you want them to be on the same page – or you could end up juggling conflicting treatment strategies.
The first step is therefore to seek out a practitioner who has a strong interest in chronic pain and an understanding of modern pain science.
A good practitioner will first take a comprehensive history, performing a thorough examination and further investigations if necessary. Importantly, they will rule out pathology and structural damage as the primary cause of pain.
Successful treatment of chronic pain relies on you being actively involved in your recovery. You are in charge. The therapist is really just a facilitator for change.

With the right support and information, you have the power to treat your own pain ultimately, you’re the one who will produce changes in your nervous system and body.
In contrast, passive interventions are things that are done to you. Be wary of practitioners who explain your pain through pathology that they propose to ‘correct’ solely with treatments like manual therapy, dry needling, surgery, injections or medications.
If you have had chronic pain for many years you will know that passive interventions such as these are not effective in the long term.
How can you find a good practitioner? Websites and practitioner profiles are a good way to learn about a therapist’s approach to chronic pain. Look for anything demonstrating their knowledge of pain science and preference for an active approach.
Prior to your first appointment, have a think about your beliefs, expectations and concerns regarding your pain, and be honest with your practitioner about these.
Ask for resources backing up the therapist’s assertions. It is good to see material from academics in the field of pain science to reassure you that their approach is legitimate and that you are receiving the best standard of care under evidence-based medicine.
My personal story with pain dragged on and eventually led me to further my understanding of chronic pain. I came across Alison Sim an osteopath with a Masters in pain science who delivers excellent education (www.beyondmechanicalpain.com). This led me to the Neuro Orthopaedic Group and their incredible text, ‘Explain Pain’ (www.noigroup.com).
Once I began reframing my knowledge of my pain I felt like I was heading in the right direction.
2. Reframe your pain
Gaining a new understanding of where your pain comes from and why it persists – in other words, reframing – is vital to treatment and will form the foundation of your recovery.

Your chronic pain, although it is physically real and debilitating, can be understood as an unhelpful protective reaction in response to perceived threat, rather than a sign of genuine danger or tissue damage (for more on this refer to part 1 and part 2)
Truly knowing and accepting this is the key part to treatment.
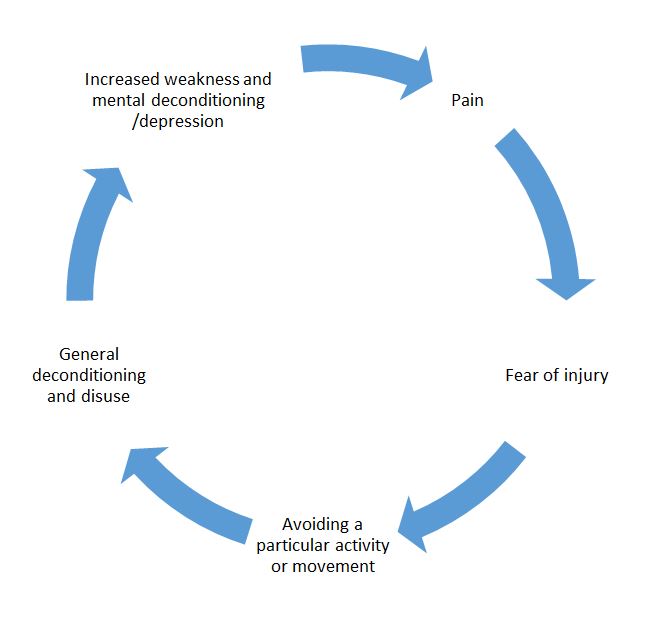
The function of pain is to alarm us in order to provoke a protective reaction and make us seek safety. However, the more scared we are of our pain, the more we inform the nervous system that the situation is very serious and deserves yet more vigilance and protection. This potentially increases our sensitivity.
This negative spiral can be avoided by reducing fear. This happens as we notice more about our pain patterns, triggers and inconsistencies, and bring awareness and acceptance to our experience of pain.
Have you noticed that your pain levels are triggered by non-physical loads (things like stress, fatigue, hormonal fluctuations and illness)? Do you feel like it comes on for unexplained reasons?

Your practitioner should help you to become aware of such triggers and patterns. It is common for pain flare-ups to happen when stress, fatigue, illness and hormonal fluctuations occur, rather than due to tissue-based load alone. This shows that the body’s perception of threat and signalling of danger are not always accurate.
You may also notice that your pain changes location and quality –another indicator that your nervous system is not perfect at discriminating or discerning threats in a precise way.
Our conscious thoughts and beliefs influence our unconscious pain response. Awareness training, or mindfulness practice, will build your skill in watching both your thoughts and bodily reactions, which can be very helpful during this hard process of reframing your pain.

With my leg pain, I greatly reduced my exercise loads (too much in retrospect – I became overly avoidant). I have always used exercise as a tool for maintaining mental health. When I lost this outlet I started a mindfulness practice, which I believe, helped me a lot.
When my pain flared up, I noticed my reaction, reflected on what was happening in my life, and weighed this up with my new understanding of my pain. This led to a new acceptance of my pain and when and why it was happening, reducing my fear of it.
You might not feel like you’re able to accept your pain right away. But even being aware of pain is a helpful step. As we decrease our fear and resistance, we loosen its grip over us and build resilience.
Returning to my personal example. I held a belief that the physical nature of my work (manual therapy) was bad for my injury and pain. Indeed, my pain was worse at work.
However, one day I realised that my leg pain was increasing when I arrived at work but before I had commenced any manual therapy. This greatly challenged my beliefs. I realised I had created a negative association between work and my pain. Unsurprisingly, my body reacted to this belief by increasing its protective response when I entered my work place.

Simply by becoming aware of this association, my pain immediately reduced.
Over time, we can come to understand and change our beliefs. We can recognise what makes us feel safe and what actions or contexts are threatening, and we can build awareness and lower our resistance and fear. All of this will help to rewire the nervous system from an unhelpful, overly sensitised state to a more stable and reliable system. Ultimately, this reverses chronic protective pain in the long term.
3. Recondition your body
From here, you are ready to set physical goals with your practitioner. Alongside rewiring the nervous system, proper treatment for chronic pain will address any physical deconditioning and build your tissue capacity.
What would you most like to return to doing? What does your condition stop you from doing? What activities are you most fearful of?

If you have been suffering for a long time, it is likely that you are physically deconditioned from avoiding activities that have provoked your symptoms or that you simply believe are bad for you. Re-conditioning, building strength and restoring movement are key.
With my disc injury, I realised I had become fearful and avoidant of forward bending. For example, I would dry my legs after a shower by raising each foot so I didn’t have to flex forward.
Therefore, one of my rehab strategies was simply to get comfortable with bending forward when drying my legs! It worked, and with various progressions I eventually made it back to more challenging forms of mobility like yoga.

One man I saw had experienced severe pain from a car accident 20 years earlier. When I first met him I was struck by how rigid and upright he was. His fear of movement was obvious, and he held a strong belief that relaxing and moving would flare up his pain.
It took time to convince him of the false association he held between movement and his pain, but after recognising and working through this belief, he was ready to start physically reconditioning.
Learning how to breathe deeply, relax his posture and stop bracing was the first priority. From there, we slowly increased his range of motion with bending and twisting movements. He was then even able to start gym training and weightlifting.
His pain levels reduced markedly but have not completely abated. However, he is able to function much more freely and has resumed activities he enjoys.
The reconditioning process can look very different for each person. Start slowly and think long term. Set achievable progressions.
One of the best things that you can do is to violate your own negative expectations. This means doing something you thought you were unable to do without causing a flare up. This builds confidence and decreases fear, breaking the cycle of pain–fear–avoidance–deconditioning–pain.
In doing this, not only are you reconditioning the body physically, but you are continuing to rewire your nervous system.
4. Trust the Process
Expect some flare-ups along the way.
After all, we are trying to reverse neuroplastic changes that have developed over months, years or decades.
Therefore, setbacks are understandable. The body has become expert at protecting you and you are actively challenging its safety mechanisms and parameters. But every setback is an opportunity to increase your resilience. Try to be mindful, stay calm, keep moving and return to the foundations of understanding your pain.
This is simple, but far from easy. You will need support, patience and courage. The path is different for each one of us. Therefore, address the threats that seem most relevant to you with priority.
For some people this will mean prioritising psychological support. For others it may be getting guidance for exercise, diet or medical management. Some people may need a bigger team around them if they have more serious medical, physical or mental complications.

As a practitioner treating patients with chronic pain, I refer to psychologists, personal trainers, doctors and other practitioners as needed.
The goal of this treatment approach is to rebuild confidence, capacity and perception of safety and to decrease perception of threat and danger.
This may seem overwhelming, especially if your pain is complicated by other diseases, hardships or constraints.
But sometimes, it does not take much.
A friend of mine finally came to see me after a 10-year history of sciatica and a history of lumbar disc injury. He does heavy work and he wanted a new set of MRI images to see if the structural damage had worsened.
Instead, I talked him through the treatment process we have outlined here and sent him away with some further pain education resources, a proposed mindfulness practice and some strength and mobility exercises.
A week later he returned and despite not having done any of his homework, his pain had miraculously resolved. This particular man has a strong mindset and I believe he was able to change his pain merely through reframing his understanding of it. Moving from a belief that his pain was an indicator of disc damage and deterioration, to an understanding that it really represented an overly sensitised nervous system was all he needed.
In the years since, he has been to see me a few times for acute episodes of lower back pain. These have resolved quickly, and together we marvel at how his chronic pain story came to a resolution merely through a new understanding of his pain.



